Do you have polycystic ovarian syndrome (PCOS)? If so, you may also have have insulin resistance. Unfortunately, the two go hand-in-hand. More on what this is—and what it means—below. But good news! Through supportive nutrition and a balanced lifestyle, you can turn insulin resistance into insulin sensitivity. Ultimately, this comes down to controlling your blood glucose. With the help of a continuous glucose monitor, you can prevent large fluctuations in glucose. And this keeps your blood sugar stable. Sayonara, insulin resistance! Today, we’re diving into the nitty gritty of blood glucose and PCOS. Hormone balance is on the horizon.

WHAT IS BLOOD GLUCOSE?
Let’s start here. Blood glucose (also called blood sugar) is our main source of energy. We get it from the foods we eat. From cereal to carrots, our body uses that sugar for energy. Our bodies break down—or convert—most carbohydrates into glucose. With the help of a hormone called insulin, glucose travels into the cells of the body where it can be used for energy. However, this doesn’t work as smoothly for a woman with insulin resistance. Instead, that sugar builds up in the blood and isn’t shuttled where it needs to go: our cells.
a pancreas in overdrive
When sugar can’t enter our cells, the pancreas pumps out more insulin. And it keeps making more insulin to get our cells to respond. Inevitably, the pancreas can’t keep up. Blood sugar keeps rising. Eventually, cells stop responding and they become insulin resistant. It’s a rather vicious cycle. However, not all hope is lost! Defeating insulin resistance is challenging, but there are ways to make the body’s cells more receptive to insulin. Along with staying active and getting proper sleep, eating balanced meals is probably the best way to combat insulin resistance.

What Is Insulin resistance?
As mentioned, insulin is a hormone produced by the pancreas. It plays a key role in maintaining normal blood glucose. And we want healthy blood glucose for many reasons. I.e. minimizing PCOS symptoms and avoiding things like the afternoon slump, feeling hangry, and a sugar crash—post-breakfast. With insulin resistance, the body’s cells don’t respond normally to insulin. In turn, glucose (sugar) can’t enter the cells as easily. So, sugar builds up in the blood. This can eventually lead to prediabetes, type 2 diabetes, PCOS, and other health conditions. Wondering if you’re insulin resistant? You can get tested with your healthcare provider. Typically, doctors will use the fasting plasma glucose test or the A1C test to diagnose prediabetes.
What comes first, PCOS or insulin resistance?
It’s nuanced, but research points to insulin resistance. Despite the fact that the signs and symptoms of PCOS begin before the signs and symptoms of insulin resistance, it is believed that insulin resistance may play a role in causing PCOS—rather than the other way around. High insulin levels, as a result of insulin resistance, stimulates the ovaries to produce more androgen hormones. Over time, this can lead to menstrual irregularity and infertility. However, controlling glucose—with the help of CGM—is particularly beneficial.
WHY IS IT IMPORTANT TO balance blood glucose if you have pcos?
Women with PCOS already suffer from conditions like irregular periods, ovaries with many cysts, excess body hair, weight gain, acne, male-pattern baldness, and infertility. Stack unstable blood glucose (insulin resistance) on top of that, and the risk for type 2 diabetes increases. Unfortunately, huge fluctuations in blood glucose makes PCOS symptoms worse. Luckily, you can minimize your PCOS symptoms—and other hormone imbalance woes, like PMS—by keeping your blood sugar in check.
MANAGE GLUCOSE LEVELS through diet
First and foremost, focus on building a balanced plate. That means including all three macronutrients: protein (animal protein or plant-based), complex carbohydrates (fruits, veggies, whole grains, beans, legumes, etc.), and healthy fats (avocados, extra-virgin olive oil, nuts, seeds, etc.). And when possible, pack in fiber-rich ingredients and fermented foods, like sauerkraut. Counter to diet culture, you also need to eat enough. Unless it’s for a short time period, constantly eating less than your caloric needs increases the production of cortisol. And chronically elevated cortisol causes blood sugar imbalance.

manage glucose levels through lifestyle
Secondly, take inventory of your lifestyle. Beyond food, managing your glucose means getting quality sleep, minimizing stress, and moving your body. Exercise is important for many reasons, but it’s crucial for helping control blood sugar spikes. Movement encourages insulin sensitivity (a good thing!). When you exercise, your muscles absorb sugar from what you eat, naturally lowering blood sugar levels. Good news: no need for intense exercise. In fact, moderate-intensity exercise—like walking—has been found to reduce blood sugar spikes. Strength training is ideal. But standing at your desk counts, too.

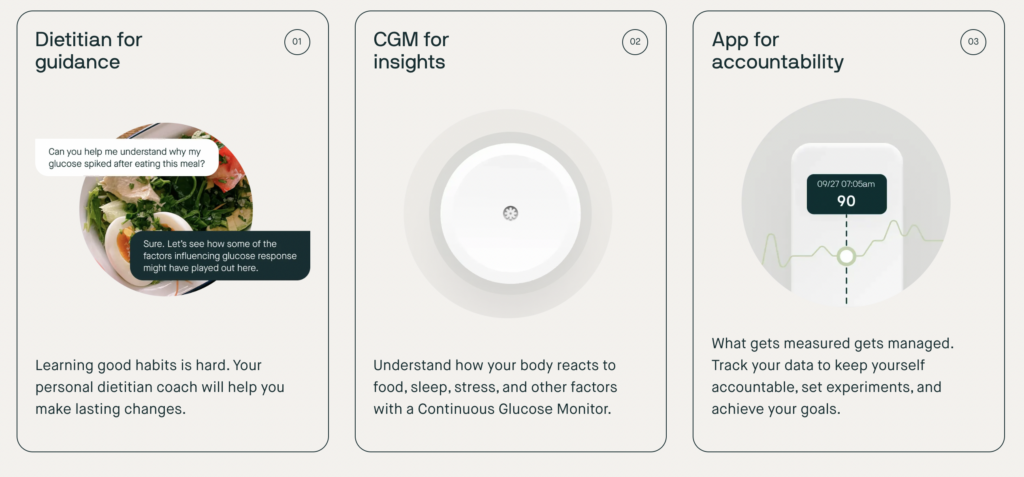
WHAT IS A CONTINUOUS BLOOD GLUCOSE MONITOR?
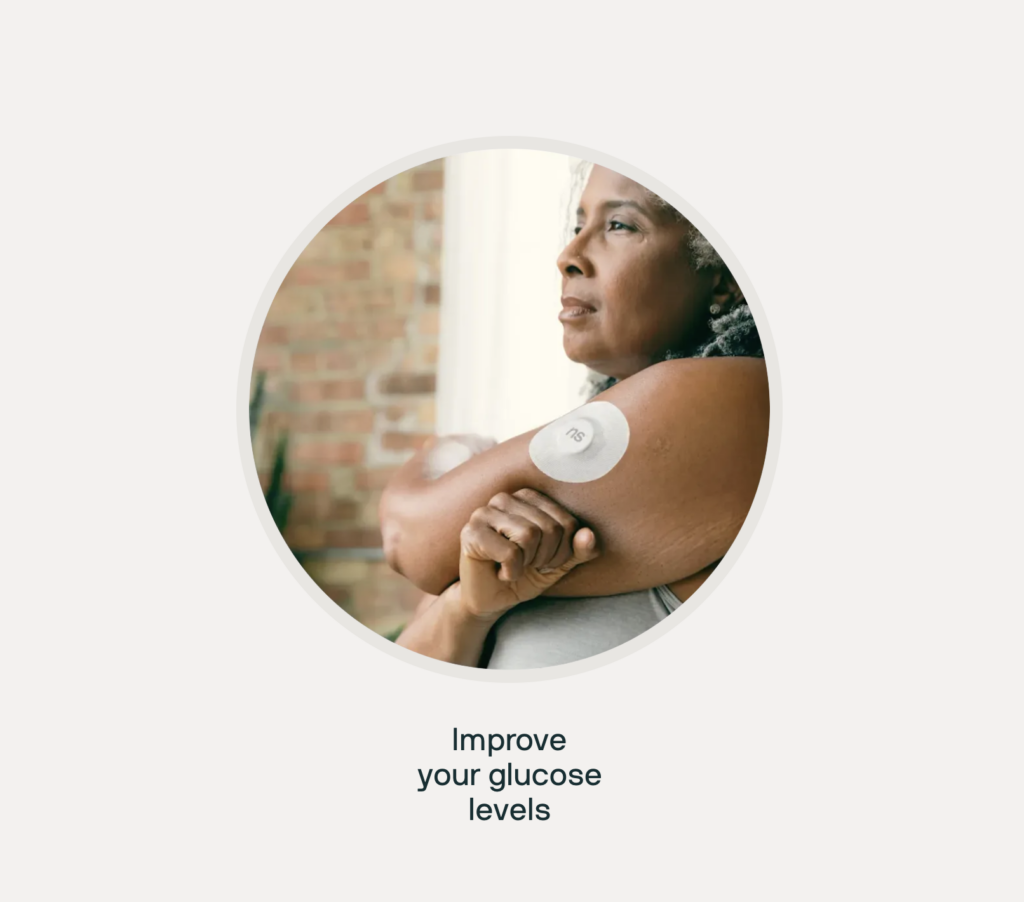
Without further ado, say hello to next-generation wellness tech: the continuous blood glucose monitor. Also known as a CGM, it’s a wearable health monitor. Like an Oura Ring, a CGM displays in-the-moment info about your health. Specifically, CGMs analyze changes in your blood glucose levels. As you live your life, your CGM is taking stats. Maybe you’ve seen social media influencers, doctors, or friends wearing a CGM censor on the back of their arm. This wearable piece of technology gives you direct insight into your health, showing how your food and lifestyle choices influence your cellular biology.

HOW IS A CGM DEVICE INSERTED?
It’s inserted under the skin on your arm via a small needle. It measures your blood glucose levels from your tissue fluid between the cells. This information is tracked every few minutes and updated to the app. Does it hurt? Nope! There may be mild discomfort when first inserting the sensor, but there is no pain afterward.
WHO ARE CGMS FOR?
They’re not just for Type 1 Diabetes (T1D). However, CGMs have been a game-changer since they were first approved by the FDA in 1999. Even if you don’t have diabetes, the CGM technology can quickly improve your overall health. CGMs help with symptoms associated with regular glucose spikes including fatigue, weight gain, imbalanced mood, metabolic / hormone issues (like PCOS), and more.
Furthermore, since regular glucose elevations are associated with an increased risk of heart disease, it can also serve as a tool to help prevent heart disease. Think of a continuous glucose monitor as the tech that allows you to lift up the hood of your car—so to speak—and see how your food and lifestyle habits impact how well your car (body) runs. With this knowledge, anyone (and everyone) can benefit from a CGM. They’re the ticket to personalized nutrition, exercise, sleep habits, and more.
THE BEST CONTINUOUS GLUCOSE MONITORS FOR 2024
So, what are the best continuous glucose monitors? I alternate between Levels and Nutrisense. In my experience, these two are the best CGMs on the market.
LEVELS HEALTH
Use this link to get yours, today *plus* two months of a free membership! Levels is phenomenal and I absolutely love wearing mine. It’s given me insights into my health stats—unlike any other wearable device. I have Levels to thank for getting my blood glucose under control!
NUTRISENSE
If I’m not using Levels, I’m using Nutrisense. Nutrisense is another app that gives you direct insight into your blood sugar levels. It’s the same sensor as Levels, just a different app you can choose from. It’s helped me improve my sleep, support my metabolism, and guide my dietary choices. While the Levels app will show you changes in your blood sugar, the Nutrisense app can also give you readings on ketone and macro values.
Want $25 off your first month with Nutrisense? Use code EDIE25 at checkout!
ARE BLOOD GLUCOSE MONITORS ACCURATE?
According to the FDA, accurate glucose meters provide results that are within ±15% of the lab 95% of the time. For example, if your lab test results show a blood glucose value of 170, your glucose meter reading must fall between 145 and 195. This is important to keep in mind when you’re using a blood glucose device. CGMs are not perfectly accurate devices either (although they are typically more accurate than standard finger pricking devices).

physical signs of blood sugar imbalance without a cGm
Even without a CGM, you’ll notice physical signs of blood sugar imbalance. For example, indications of blood glucose spikes include immediate energy, adrenaline, etc. Dips in blood sugar include hanger, shakiness, and foggy brain. These are all helpful and insightful. But CGMs are much more specific. Over time, you can track your glucose patterns and responses to certain foods and habits. These patterns can help you improve insulin sensitivity, reverse pre-diabetes and type 2 diabetes, improve pregnancy outcomes for gestational diabetes, minimize PCOS symptoms, and more.
If you don’t want to wear a CGM, check out my Blood Sugar Reset Meal Plan. It’s an intro to managing blood sugar, complete with a a 7-day meal plan to help balance your blood sugar.

This article is for informational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and we recommend that you always consult with your healthcare provider.


Leave a Reply