Do you struggle with intense PMS symptoms, PCOS, or an irregular period? If so, it’s time to learn how blood sugar impacts your menstrual cycle. Spoiler alert: they’re closely knit. Whether you’re entering your mid-30s, or menopause is around the corner, your diet can make or break hormone health. Unfortunately, consuming too many ultra-processed foods, inflammatory oils, and sugars sets you up for a hormonal fiasco. But good news! The solution lies in your eating habits. When it comes to a normal menstrual cycle (and improving fertility), understanding blood sugar and ovulation is key. Use food as medicine to bring your body into balance—one grocery basket at a time.

WHAT IS BLOOD GLUCOSE?
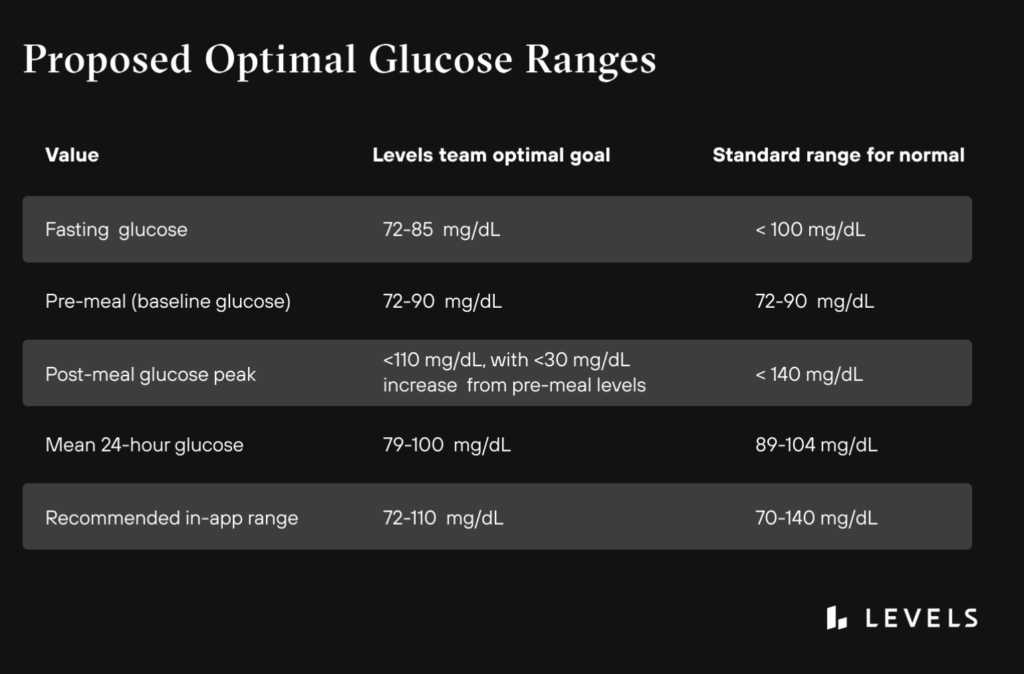
Let’s start here. Blood glucose (also called blood sugar) is our main source of energy. We get it from the foods we eat. From cereal to carrots, our body uses that sugar for energy. Our bodies break down—or convert—most carbohydrates into glucose. With the help of a hormone called insulin, glucose travels into the cells of the body where it can be used for energy. However, this doesn’t work as smoothly for a woman with insulin resistance. Instead, that sugar builds up in the blood and doesn’t shuttled where it needs to go: our cells.
What happens As blood sugar Rises?
When sugar can’t enter our cells, the pancreas pumps out more insulin. And it keeps making more insulin to get our cells respond. Inevitably, the pancreas can’t keep up. Blood sugar keeps rising. Eventually, cells stop responding and they become insulin resistant. It’s a rather vicious cycle—that also impacts your period. However, not all hope is lost! Defeating insulin resistance is challenging, but there are ways to make the body’s cells more receptive to insulin. Along with staying active and getting proper sleep, eating balanced meals is probably the best way to combat insulin resistance.

How to become insulin sensitive
When your blood sugar is chronically high, your body slowly becomes less sensitive to insulin. This is known as insulin resistance. And it isn’t the goal. Instead, you want to be insulin sensitive. Unfortunately, when you’re insulin resistant, it takes more and more insulin to shuttle circulating glucose into your cells. In turn, this causes blood sugar imbalance and a host of menstrual cycle imbalances. How to become insulin sensitive: prioritize a healthy breakfast, get quality sleep (7-9 hours), walk after eating, add more colorful produce to your plate, reduce your intake of added sugars, and aim for 20+ grams of high-quality protein per meal.
See here for my blood sugar-friendly / hormone-balancing meal plan.
Does INSULIN RESISTANCE cause hormone imbalance?
It’s nuanced, but research says yes. Despite the fact that the signs of hormone imbalance typically begin before the symptoms of insulin resistance, it is believed that insulin resistance may play a role in causing menstrual cycle issues. High insulin levels, as a result of insulin resistance, stimulates the ovaries to produce more androgen hormones. Over time, this can lead to menstrual irregularity and infertility. However, controlling glucose (through diet, lifestyle, and the help of CGM!) is particularly beneficial.
Blood Sugar and your menstrual cycle
So, how does blood sugar relate to your menstrual cycle? Study after study shows that blood sugar impacts all female sex hormones. When insulin is elevated—aka blood sugar levels are high—it puts stress on the body. This causes a spike in cortisol, and this spike has a ripple effect on other hormones. Since progesterone and testosterone compete for the same receptor sites, high cortisol causes low progesterone. This leads to symptoms like heavy periods, migraines, anxiety, acne, PMS, estrogen dominance, endometriosis, and more.

How Elevated Blood Sugar Impacts Ovulation
Additionally, your ovaries also have insulin receptors! Meaning, elevated insulin can cause the ovaries to produce more testosterone. This ultimately impacts—or entirely stops—ovulation. It causes issues like PCOS and irregular periods. Elevated insulin also lowers SHBG (sex hormone-binding globulin), which contributes to both high estrogen and testosterone. In turn, causing symptoms like tender breasts, heavy periods, and uterine fibroids.
Why ovulation is important
FYI: it’s not just to make a baby! Ovulation is beneficial because it’s how we, as women, make hormones. It provides the body with much-needed levels of estrogen and progesterone—hormones that play a role beyond fertility. Every month, as the ovaries get ready to release an egg, they release estrogen. Estrogen, in turn, stimulates serotonin, which is why women often feel more outgoing, social, and energetic in the days leading up to ovulation. Mood aside, ovulation is an important catalyst in a woman’s cycle. Not ovulating can eventually result in issues with bone density, metabolism, mental health, and more. Not sure if you’re ovulating? Use LH strips!

Your Menstrual cycle and Blood Sugar
As women, the natural ebbs and flows of our hormones affect blood sugar (and insulin sensitivity). Curious to know what’s happening to your blood sugar—in relation to your menstrual cycle? Let’s dive into the entire cycle, starting with the first day of your period.
Days 1-7
Your Period
Hello, period! You may experience higher blood sugar levels and insulin resistance on the first few days, but insulin sensitivity should revert back to normal for the rest of your period, and a few days after it ends.
Days 11-14
Follicular phase
During ovulation, you may experience higher (and somewhat erratic) blood sugar levels and insulin resistance. As your body prepares to release an egg, hormones rise, which can cause a spike in your blood sugar. This lasts 2-3 days.
Days 15-20
Ovulation
Blood sugar typically balances itself out (with the support of proper nutrition) at the start of the luteal phase.
Days 21-28
Luteal Phase
This is the point in your cycle, because of what’s happening with your progesterone, you’re more likely to experience insulin resistance and higher blood sugar levels. This isn’t uncommon before your period starts again. During this time, prioritize healthy fats, protein, and fiber with each meal. Take a look at my hormone balancing meal plan for ideas and inspiration.
Keep in mind that every woman’s cycle is different, and it is normal for lengths to vary. Your cycle may be longer or shorter than the phases listed above.

Hormone balance ebook
Ready to take the next step in your hormone-healing journey? Grab your copy of Master Your Menstrual Cycle—my holistic guide to balancing your hormones with ease. Available for only $15!
Images courtesy of Unsplash. This article contains affiliate links. Thank you for supporting Wellness with Edie. This article is for informational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and we recommend that you always consult with your healthcare provider.


Leave a Reply